Editor’s Note: The content of this article includes mention of sexual assault.
“Whore.” “Slut.”
These were two words one Elon University student was called when she shared with potential sexual partners that she has a sexually transmitted infection. Martha, whose name has been changed to protect her privacy, tested positive for HSV-2 — more commonly known as genital herpes — after she was sexually assaulted as a young teenager.
“I’ve been told things like, ‘Oh, I didn’t know you were one of those,’” Martha said. “‘You're definitely a college girl.’ Those kinds of things, like really mean things.”
After her diagnosis, when Martha wanted to have sex with other people, she more often than not was looked at with judgment. She said this caused her to internalize the guilt and shame she felt.
“What if I never get to have sex?” Martha said. “I was still in that mindset of ‘Maybe I don’t deserve sex.’”
Elon Medical Director of Student Health and university physician Dr. Ginette Archinal said Martha’s guilt and shame are not unusual. When Archinal tells students they have tested positive for a sexually transmitted infection, especially genital herpes, emotions are often high.
“Tears, crying, upset, fear. Fear about, ‘What's it going to mean in the future?’” Archinal said. “Anger towards the person who may have given them the STI, anger to direct it inward for a perception of carelessness.”
Martha is not alone. According to the Centers for Disease Control and Prevention, one in five Americans have an STI. People ages 15 to 24, like Martha, are more susceptible to contracting STIs as opposed to older Americans.
According to Archinal, Elon Student Health diagnoses hundreds of STIs every academic year, the most common ones being chlamydia and genital herpes. The recent spike in chlamydia mirrors national trends.
According to Archinal, 70% of people on Elon's campus who test positive for herpes request a follow-up, in-person visit to get advice about how to disclose the STI to sexual partners and friends.
Archinal tells students to communicate openly and honestly with their partners.
“If you are comfortable enough to be having sex with somebody, that's a very intimate relationship,” Archinal said. “If you are not comfortable enough to talk to that person about your previous sexual experience and any infections involved, you probably shouldn't be having sex with them.”
But she understands that can be difficult so she advises students to use their own discretion.
In the U.S., according to the CDC, regulations about disclosing STIs depend on the state and the circumstances under which the STI was contracted. In North Carolina, state law requires someone with chlamydia to notify all sexual partners from 30 days before the onset of symptoms. People infected with human immunodeficiency virus, or HIV, are required to disclose their HIV status to past and future sexual partners, although some exceptions apply.
Martha said she has disclosed her genital herpes to every potential sexual partner she’s had. She said some people have called her names, but others have given her positive responses. She appreciates people who are direct right off the bat.
“That's the best-case scenario. If you're not comfortable just telling them right away. Ghosting, saying mean things, is never kind,” Martha said. “If you're not comfortable, you're not comfortable, and just let someone know.”
Elon junior Leah Short is the team lead for the sexual health focus group in SPARKS peer educators. The peer health education group leads workshops about sexual health education and hosts events across campus. Short said STI disclosure is about personal responsibility.
“Automatically disclosing that information is really important,” Short said. “One, because you don't want to expose or transmit the STI to someone else. I think that honesty and having that conversation goes along with that.”
Short’s team hopes to normalize conversations about sex. Martha said disclosing to potential partners could be hard, especially if her news was not well received. That’s why Martha found it easier to disclose and date people who also have an STI. There are a handful of websites for those living with STIs to navigate their dating world. Martha used a website called Positive Singles and found it much more relaxing.
“The fact that they already had genital herpes made me feel a lot more comfortable because even if someone did feel totally comfortable having sex with me, there's still that voice in the back of my mind that's like, ‘You shouldn't do it. You don't deserve to infect this person,’” Martha said.
Eventually, Martha decided to give Tinder a try — that’s where she met her current boyfriend. He doesn’t have genital herpes and she hasn’t had an outbreak since they have been together. An outbreak is when genital sores resurface after the initial symptoms.
Martha also had to work through telling her friends. She remembers the support she got from one of the first people she told.
“I was still worthy of love and a relationship and that there's nothing wrong with me for having a STI,” Martha said. “Just receiving that affirmation was really great.”
Beyond initial disclosure, the STI has the potential to be brought up again among friends. Archinal is adamant that laughing, poking fun or making jokes about someone’s STI is not acceptable.
“I do not know why anybody would find that amusing. Honestly, if somebody confides in somebody something about any health issue and that person they're confiding in thinks is a joke, walk away from that person because they are not your friend,” Archinal said.
Martha said making jokes about STIs is a “social jumping hoop.” She, “airs on the side of no joke” but it, “depends on how close you are to that person.”
She said she often mirrors the body language and tone of the other person.
“I would say that depends on how close you are to that person and when they disclosed. If they've just told you and they're pretty upset, look pretty shaken, maybe not a joke, maybe not appropriate,” Martha said.
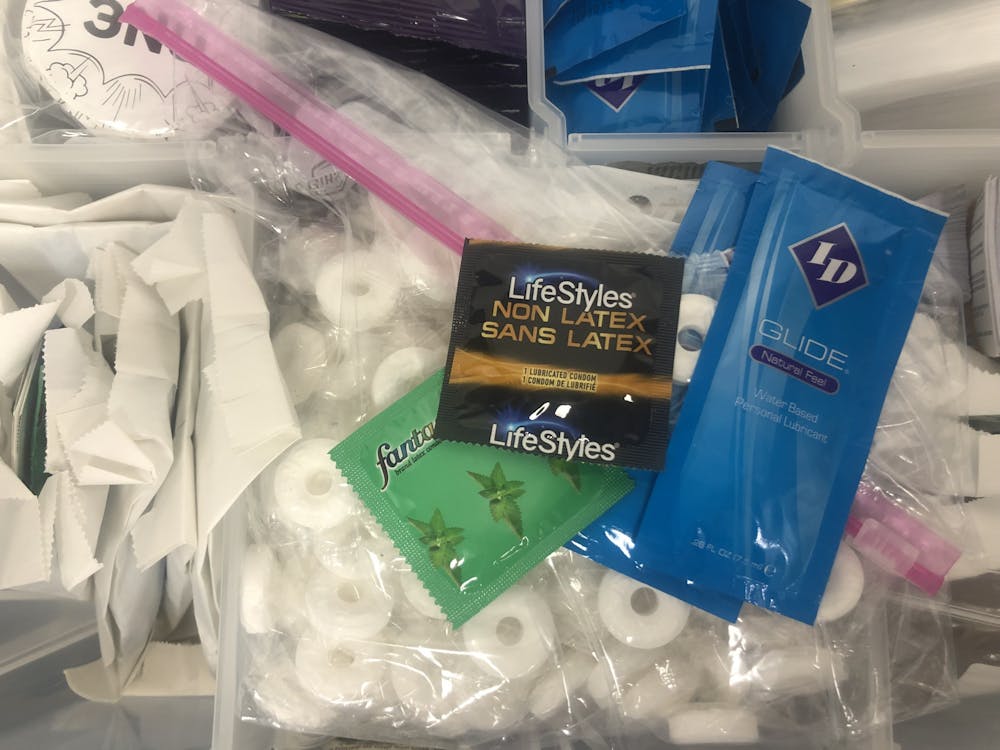
Archinal said getting tested for STIs followed by open and honest communication with sexual partners is the best way to prevent STIs. She encourages students to share negative test results before having sex, agree to be monogamous and avoid alcohol or any other recreational drugs in sexual situations. She advocates for using barrier methods including condoms during any type of sex since STIs can be spread through kissing and oral sex, along with penis ejaculation into a vagina or anus. Students can access safer sex supplies using SPARKS’s Protect Direct service. Students can request free safer sex supplies to their campus box.
Testing is another way to prevent the spread of STIs. Students can make an appointment at student health services. STI tests at student health services are an out-of-pocket expense that range from $8 to $44. But student health can provide a receipt so that anyone who wants to file with insurance can be reimbursed. Archinal said health providers at student health services are careful to use language that does not cast shame or judgment when talking to students about test results to eliminate shame or stigma.
“The last thing people need is for somebody to say, ‘Well, of course, if you'd use condoms every time like I told you to…’ Nobody needs to hear that,” Archinal said.
STI testing is also available at urgent care clinics and private medical offices. There are also home test kits that are available at pharmacies. Tests at the Alamance County Health Department are free.
If students test positive for a STI, Archinal said students may be prescribed medicine to treat the symptoms. These prescriptions are covered by insurance. Archinal said if students cannot afford treatment then the STI clinic at the health department is the best resource to help.
When it comes to emotional support, Archinal said the provider who diagnoses the student can answer questions and offer support. Beyond that, she said confiding in parents can be helpful.
According to its website, staff at university counseling services are prepared to help students with a host of concerns, including romantic partners and interpersonal issues.
“If you have a bad experience when you're disclosing, don't bottle it up,” Archinal said. “Talk to somebody that you trust is going to keep it private.”